It has been established that so-called deep brain stimulation can be a powerful remedy for people that suffer from treatment-resistant depression that can't be remedied with conventional methods. However, it is not precisely known how it works.
Scientists around the globe have been hurrying to get this innovative treatment optimized and authorized so that it can be applied to people in need. However, to determine its effectiveness, they need to ascertain an objective biomarker.
A new study published in the journal Translational Psychiatry has defined such a biomarker and provides some fascinating insights on how deep brain stimulation reduces symptoms of depression.
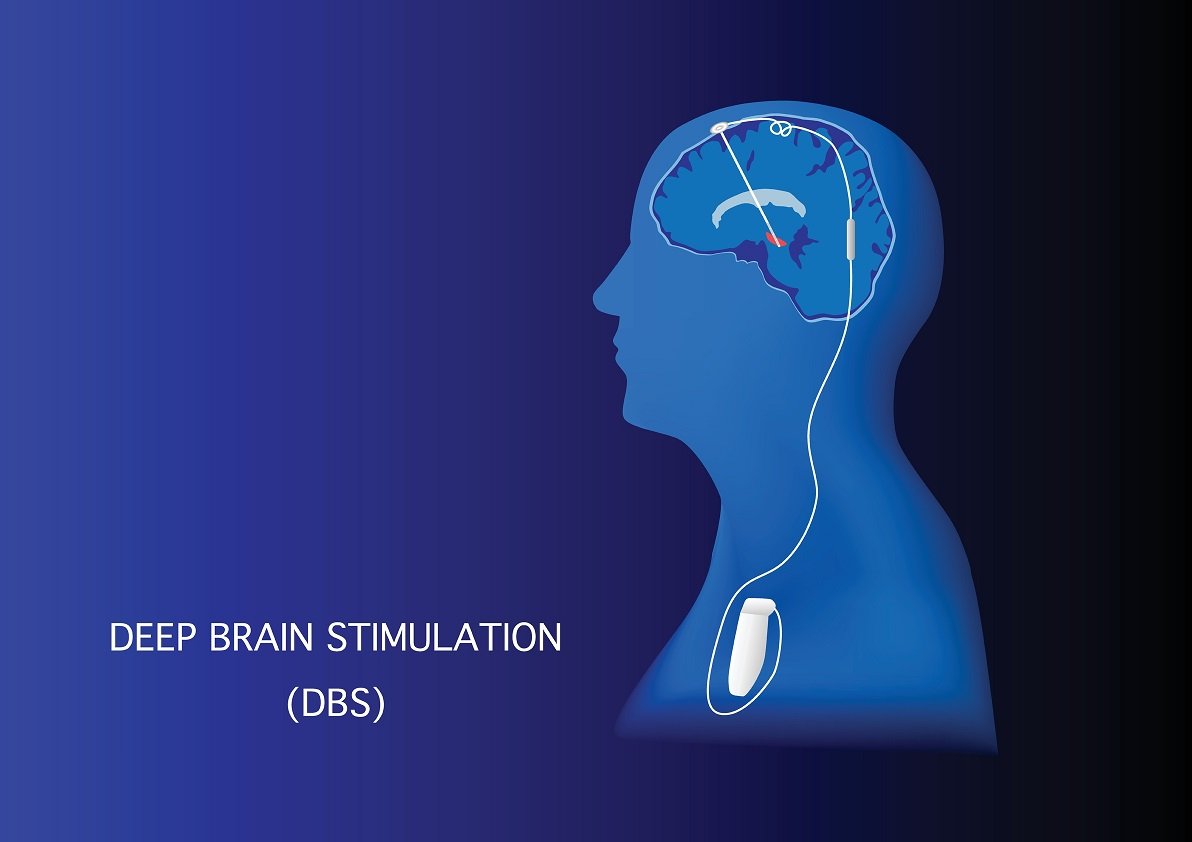
Image Credit: Vectorium via Shutterstock
What is deep brain stimulation?
Deep brain stimulation, or DBS for short, is a neurosurgical technique that involves implementing a medical device called a neurostimulator. The neurotransmitter transmits electrical pulses through implanted electrodes aimed at specific targets in the brain or the treatment of a variety of disorders such as Parkinson's disease and OCD. Some people perhaps aptly refer to it as a "brain pacemaker" due to the way it operates. (Consider exploring the sources and further reading section below this article for more details)
Deep brain stimulation in depression
Currently, DBS has been authorized by the FDA for treating Parkinson's disease, essential tremors, OCD, and epilepsy. However, it is still considered an experimental treatment when it comes to treating depression.
Nonetheless, DBS has frequently been shown to be a favorable treatment over a period of six months for those who suffer from depression who inadequately respond to standard treatments.
Although the potency of deep brain stimulation combating depression has been shown multiple times, scientists observed dissimilarities between patients regarding recovery times.
Comprehending the processes behind these first quick and repeatable behavioral effects, as well as their involvement in forecasting more essential long-term response trajectories, will be critical to adequate treatment.
Image Credit: Teeradej via Shutterstock
Why deep brain stimulation can be effective in treating movement disorders
Dr. Allison C. Waters, a co-first author of the study, explained that she and her team noticed a change in the beta brain waves within minutes of stimulation inside the operating room.
According to Waters, beta brain waves are commonly connected with the "brain's determination of whether to stop or keep going with a course of action." This is why DBS can be effective against movement disorders such as Parkinson's disease.
No clear brain signal for depression
Whereas there is an obvious brain signal related to movement disorders, there is no clear signal to target for depression.
Co-first author, Mohammad Sendi, asserted that the team was able to use machine learning and AI to investigate hidden alternations in brain status that may explain the evident behavioral changes that have been observed.
The study
In their study, the researchers took a look at eight patients suffering from treatment-resistant depression via an electrophysiological recording that was taken place during the implantation of the neurostimulators.
Before the patients underwent the operation, researchers identified the optimal target within an area in the brain that has been thought to play a major role in depression.
The scientists then used machine learning to find the differences between the pre-recorded baseline and the first exposure to stimulation during the operation. Spectral inputs were then assessed and classified as predictors of depression reduction.
After a single week, a reduction in depression scores by 45.6 percent was observed. This response correlated with a decrease in the SCC LFP beta power, which contributed most to classifier success. Thus, confirming reduction in beta power as a new biomarker for DBS treatment optimization.
Depression relief within minutes, not months
Lead author DR. Helen S. Mayberg remarked that the treatment of depression is commonly thought of as a process that takes months before achieving significant and stable improvements. But her team's research demonstrates reproducible and consistent changes in a brain readout over the first minutes of optimized stimulation.
The study presents a new mechanistic understanding of the so-called 'depression switch' that moves a patient from a state of sustained mental immobility and pain to relief and the restored capability to move and engage.
As Dr. John Ngai, director of the NIH BRAIN Initiative, put it: ''This research provides individuals who have struggled with depression a sense of hope through advancements in existing technology.''
As this study shows, tremendous advancements are being made in the comprehension of mental health illnesses. We are excited for further improvements for those suffering from these horrible conditions.
Be sure to check out the paper listed below for more details about how the study was performed.
Sources and further reading:
Intraoperative neural signals predict rapid antidepressant effects of deep brain stimulation (Translational Psychiatry)
DBS for TRD With the Medtronic Summit RC+S (U.S. National Library of Medicine)
Deep brain stimulation (Johns Hopkins Medicine)
Diagnosis and definition of treatment-resistant depression (National Library of Medicine)
What are Biomarkers? (NCBI)
If you enjoy our selection of content, consider subscribing to our newsletter - (Universal-Sci Weekly)
FEATURED ARTICLES: